One Health Action has recently been highlighted in the report released by the Organisation for Economic Co-operation and Development (OECD) on the health and economic costs of antimicrobial resistance (AMR).
About OECD Report:
- The report “Embracing a One Health Framework to Fight Antimicrobial Resistance” has given necessary recommendations to combat AMR.
- It was built on the statistics from OECD, European Union (EU) and European Economic Area (EEA) countries and Group of 20 (G20) countries.
Key highlights of the report:
Antibiotic Consumption Trends:
- The total consumption of antibiotics in humans has been increasing for the last two decades, modestly across OECD, EU/EAA, and G20 countries.
- It is suspected to remain steady in OECD countries between 2015 and 2035.
- Among EU/EEA and G20 countries, the total consumption could decline to 3.3% and 6.2%, respectively.
- At present, it is 20% in OECD countries, 22% in the EU/EEA, and 30% in the G20 countries.
Last-Resort Antibiotics and Resistance:
- Consumption of last-resort antibiotics (like polymyxins) has increased faster as compared to the total consumption.
- Last-resort antibiotics are used to treat infections with bacteria resistant to the common antibiotics or, in cases of severe infections, where an effect must be ensured.
Antibiotic Usage in Animals:
- The average sales of all classes of antibiotics have declinedglobally between 2000 to 2019.
- It is halved in OECD countries from 181 to 91 milligrams of antimicrobials per kilogram of food animal.
- Antimicrobial consumption in animals may fall by 10% in OECD countries between 2020 and 2035.
- By 2035, the sale of veterinary antimicrobials in G20 countries could nearly double that of the sales in OECD countries.
- The resistant proportions for 12 priority antibiotic-bacteria combinations stood at 20% in 2019.
- One in every five infections in OECD and EU/EEA are due to antimicrobial-resistant organisms.
Regional Antibiotic Resistance and Future Projections:
- Resistance to third-line antibiotics could double in 2035 than in 2005 if action is not taken.
- In 2019, the resistance proportions were above 44% for India, Greece and Türkiye, and are estimated to remain high till 2035.
- 90% of infections can be resistant to antibiotics, like fluoroquinolone-resistant and carbapenem-resistant Acinetobacter baumanii in countries with high resistance proportions.
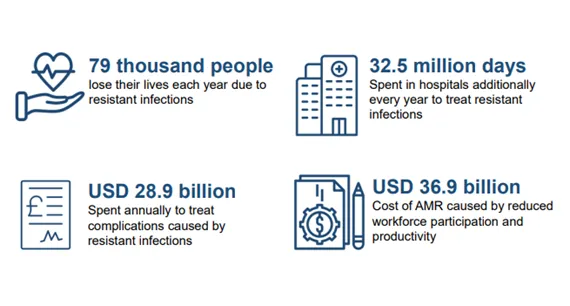
Impacts of AMR on Health and Economy:
Health:
- AMR causes around 79,000 deaths every year, which is 2.4 times more than diseases such as influenza, tuberculosis and acquired immunodeficiency syndrome (AIDS) in 34 OECD, and EU/EEA countries.
- More than 4.3 million infections have been reported, mostly in people above 65 years of age.
- 75% of AMR-related deaths are mainly caused by Escherichia coli, Klebsiella pneumonia and Staphylococcus aureus.
- These are responsible for one in three resistant infections.
- Healthcare-associated infections (HAIs) constitute about one-third of all resistant infections and account for 60% of all deaths.
- Every year around 32.5 million additional days are spent in hospitals due to resistant infections (As high as the entire acute bed capacity in a small country like Spain).
Economy:
- Healthcare systems are burdened with a huge cost of around $28.9 billion each year up to 2050 for 34 OECD and EU/EEA countries.
- The total annual cost ofAMR across 34 OECD and EU/EAA countries is around $58 per capita.
- One-third of it is due to increased health expenditure while remaining is due to reduction in productivity of workforce.
- 47 out of total 51 OECD, EU/EEA, and G20 countries have national action plans but only 10 countries have incorporated financial provisions.
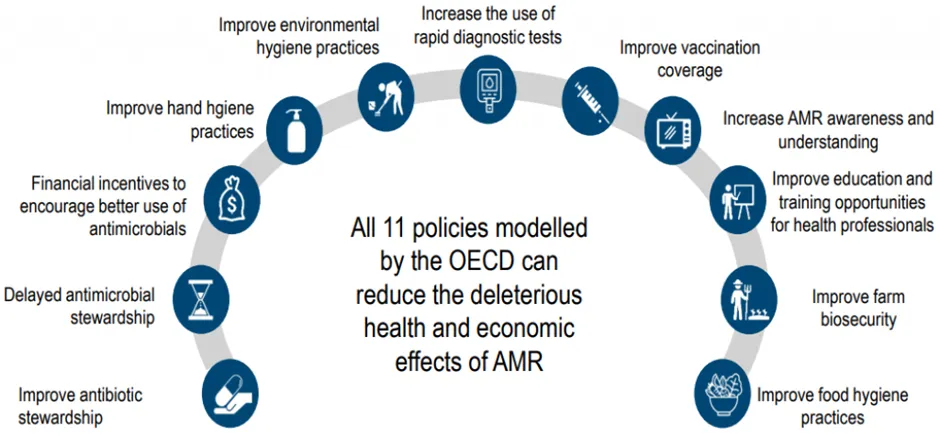
Prevention of AMR through One Health:
- AMR can be tackled by considering 11 one health policy interventions.
- Hospital-based intervention plans: It focuses on hand hygiene, environmental hygiene, and scaling up antimicrobial stewardship plans.
- Community-based intervention: This includes delayed antibiotics prescription, financial incentives, scaling up the use of rapid diagnostic tests, mass media campaigns and prescriber training.
- For most interventions, benefits and gains made in health expenditure and productivity of the workforce are much more than the costs of implementing these measures.
- The return on investment (ROI) ratio ranges from 2.3 to 24.6 in different policy measures.
- OECD has considered three policy packages including a hospital-based package, a community-based package and a mixed package.
Mixed Health package:
- It includes hand hygiene, scaling up antimicrobial stewardship programs, delayed antimicrobial prescription, increasing the mass media campaigns, biosecurity of farms, and enhancing the food handling practices.
- The investment in this package could combat more than 1.6 million infections every year and approximately 17,000 deaths.
- It saves costs in health expenditure and gains through the involvement of workforce and productivity.
- The annual average cost of implementing it is around five times lower than the reduction in health expenditure and productivity gains combined.
About Antimicrobial Resistance (AMR):
- AMR is caused due to the overuse and misuse of antibiotics which makes micro-organisms resistant to them.
- It is accepted as a global public health issue, leading to a silent pandemic.
- It could result in extended hospitalisations and increased pressure on healthcare systems.
About the Organisation for Economic Co-operation and Development (OECD):
- The OECD is an intergovernmental organisation with 38 member countries, founded in 1961 to stimulate economic progress and world trade.
- It is recognised as a highly influential publisher of mostly economic data through publications as well as annual evaluations and rankings of member countries.
- India is not a part of the OECD.
Ref: Source
| UPSC IAS Preparation Resources | |
| Current Affairs Analysis | Topperspedia |
| GS Shots | Simply Explained |
| Daily Flash Cards | Daily Quiz |